The Deep Painful Bumps: A Complete Guide to Nodulocystic Acne
Struggling with deep, painful acne bumps? Learn about nodulocystic acne causes, effective treatments from dermatologists, and prevention tips to reduce scarring.

We’ve all been there. You feel a tiny, tender spot beneath the skin and hope it will just go away. But instead, it swells into a large, red, angry bump that hurts to the touch. It doesn’t come to a head like a normal pimple, and it seems to stick around for weeks. If this sounds familiar, you might be dealing with a type of severe acne known as nodulocystic acne.
This isn't your average whitehead or blackhead. It’s a different beast altogether. Because it’s so deep and inflamed, nodulocystic acne carries a high risk of permanent scarring and can be frustratingly resistant to the over-the-counter washes and creams you find at the drugstore.
The goal of this article is to be your friendly guide through this tough skin condition. We’ll break down exactly what it is, why it happens, and—most importantly—what actually works to treat it. We’ll separate fact from fiction, explain how different treatments work (and their side effects), and give you the knowledge you need to have an informed conversation with a dermatologist. Let’s get started.
What is Nodulocystic Acne? Understanding the Beast
To understand nodulocystic acne, you first have to understand how normal skin works. Think of your skin as having millions of tiny drainage pipes (follicles) that bring oil (sebum) from deep down to the surface to keep your skin lubricated.
In regular acne, these pipes get clogged with a mix of dead skin cells and oil. This creates a comedo—either a blackhead (open plug) or a whitehead (closed plug). If bacteria get involved, the area becomes red and inflamed, creating a papule or pustule (the classic pimple).
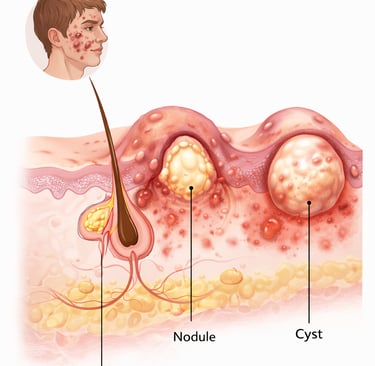
Nodulocystic acne is when this system fails spectacularly and deep underground. The name is a combination of two things:
Nodules: These are hard, painful lumps that form deep within the dermis (the skin’s middle layer). They happen when a follicle wall ruptures far beneath the surface, spilling oil, skin cells, and bacteria into the surrounding skin. This triggers a massive, deep inflammatory response. Because they are so deep, they feel like hard, tender knots.
Cysts: These are similar to nodules, but they are soft, fluid-filled sacs. They form when the body tries to build a wall around the deep infection to keep it from spreading. These are the large, soft, pus-filled bumps that can be incredibly painful.
Most people with this condition have a mix of both, hence the combined term. These lesions are large (often more than 5 millimeters across), painful, and can take weeks or even months to heal. Because they destroy healthy skin tissue so deeply, they are the primary culprits behind acne scars.
The Perfect Storm: What Causes Nodulocystic Acne?
So, why does this "perfect storm" happen in some people and not others? It’s rarely one single thing, but rather a combination of factors.
The Four Key Players
Oil Overproduction: Your sebaceous glands, stimulated by hormones, pump out too much oil. This is the "fuel" for the fire.
Clogged Pipes (Follicular Hyperkeratinization): Normally, dead skin cells are shed from the follicle opening. In acne-prone skin, these cells are shed too quickly and stick together, forming a plug. Think of it as a drain clogged with hair and grease.
Bacteria (Cutibacterium acnes): This bacteria lives on everyone’s skin. It’s not an "infection" in the contagious sense. However, when the follicle is clogged and filled with oil, this bacteria, which prefers low-oxygen environments, thrives. It triggers inflammation by releasing enzymes and attracting immune cells to the area.
Inflammation: This is the body’s response to the rupture and the bacteria. In nodulocystic acne, this response is extreme. It’s what causes the deep, red, painful swelling.
Genetics: The Hand You Were Dealt
This is a big one. You didn't do anything to cause this. If your parents or siblings had severe, scarring acne, you are much more likely to have it too. Your genes influence how much oil you produce, how your skin cells shed, and even how your immune system responds to C. acnes bacteria. In some cases, it’s not just the amount of bacteria, but the specific "bad" strains you might be genetically prone to harboring that can trigger this severe inflammatory reaction.
Hormones: The Internal Trigger
Androgens, like testosterone, are the main hormones that rev up your oil glands. This is why acne explodes during puberty. But for adults—especially women—hormonal fluctuations during menstrual cycles, pregnancy, or menopause can also trigger deep breakouts. Stress is another factor because your body produces more cortisol (the stress hormone), which can also ramp up oil production.
External Factors: Fuel on the Fire
While they don't "cause" the condition on their own, certain things can make it worse:
Anabolic Steroids: Used by some bodybuilders and athletes to build muscle, these are synthetic hormones that can trigger severe, explosive nodulocystic acne.
Pressure and Friction: Anything that repeatedly rubs against the skin, like a backpack strap, helmet, or even a cell phone, can aggravate the follicles and trigger breakouts in a susceptible person.
Who Gets Nodulocystic Acne?
While anyone can get a deep pimple now and then, nodulocystic acne is most common in:
Young Men: Due to higher levels of androgens, teenage and young adult men are more frequently affected.
Adults with a History: It can persist or even start in adulthood, particularly in women dealing with hormonal issues.
People with a Family History: As mentioned, genetics play a massive role.
The Doctor’s Visit: Diagnosis and When to Seek Help
Here’s the most important takeaway: You cannot treat nodulocystic acne on your own. If you have large, painful bumps under your skin, it’s time to see a professional—ideally a board-certified dermatologist.
A dermatologist can diagnose this condition just by looking at your skin. They will assess the types of lesions, their depth, and the areas affected. They will also ask about your family history and any triggers you've noticed.
Seek help immediately if:
Over-the-counter products haven’t worked after a few weeks.
Your breakouts are painful.
You notice you're starting to scar or get dark spots after pimples heal.
Your acne is making you feel anxious, self-conscious, or depressed.
Battling the Breakouts: Treatment Options Explained
Treating nodulocystic acne is a bit like putting out a house fire—you need more than a spray bottle. It requires a strategic, multi-pronged approach from a professional. Here are the main weapons in a dermatologist's arsenal, broken down so you can understand what they do.
1. Oral Medications: The Heavy Hitters
Because the problem is deep within the skin, topical creams often can't reach it. Oral medications work from the inside out.
Isotretinoin (Formerly Known as Accutane)
This is the closest thing we have to a "cure" for severe, nodulocystic acne. It’s a powerful oral retinoid (a high-dose form of Vitamin A).
How it works: It’s the only treatment that targets three of the four main causes of acne. It shrinks oil glands (reducing oil by up to 90%), normalizes skin cell shedding (keeping pores unclogged), and has strong anti-inflammatory effects.
Effectiveness: Extremely effective. After a standard course of 20-28 weeks, most patients experience complete or near-complete clearance, often permanently.
Timeline: You’ll usually start seeing improvement in 1-2 months, but the full course is needed for the best results.
Side Effects: They are significant and require careful monitoring.
Common: Severe dryness of the lips, skin, eyes, and nose (nosebleeds). Muscle and joint aches are also common.
Serious: It causes severe birth defects, so women of childbearing age MUST use two forms of birth control and have monthly pregnancy tests before, during, and after treatment. This is not optional.
Mental Health: There has been concern about links to depression and suicide. While research is mixed, current medical guidelines stress that patients should be counseled about this and monitored for mood changes before and during treatment.
Other Risks: It can raise cholesterol and liver enzymes, requiring regular blood tests.
Who Should Consider It: Patients with severe, scarring, nodulocystic acne that hasn't responded to other treatments. It is a strictly regulated medication that requires close dermatologist supervision.
Oral Antibiotics (e.g., Doxycycline, Minocycline)
How they work: They reduce the population of C. acnes bacteria and, importantly, have powerful anti-inflammatory effects.
Effectiveness: They can be very effective at calming down a bad flare-up.
Timeline: You may see improvement in 4-6 weeks.
Limitations: They are generally not a long-term solution because bacteria can become resistant. They are often used as a bridge to another treatment or alongside topicals.
Side Effects: Can include stomach upset, sun sensitivity (you will burn very easily!), and for minocycline, dizziness or rare skin pigmentation.
Drug Interaction Warning: Doxycycline can make birth control pills less effective. Always use a backup method and inform your doctor of all medications you are taking.
Hormonal Therapy (For Women)
Options: Combined oral contraceptives (the pill) or spironolactone.
How they work: They block or regulate androgens, the hormones that stimulate oil production.
Effectiveness: Can be highly effective for women whose acne flares around their period or is driven by hormonal imbalances.
Timeline: It can take 3-6 months to see the full effect.
Side Effects: Vary by the specific medication but can include nausea, breast tenderness, and mood changes.
2. In-Office Procedures: Targeted Strikes
These are treatments your dermatologist can perform to tackle individual cysts or overall inflammation.
Intralesional Corticosteroid Injections
What it is: The dermatologist injects a diluted steroid solution directly into a large, painful cyst or nodule.
How it works: The steroid rapidly reduces inflammation.
Effectiveness: Extremely effective for individual lesions.
Timeline: You'll see significant flattening and reduced pain within 24 to 48 hours.
Who Should Consider It: Anyone with a few isolated, painful, giant bumps that won't go away. It’s a quick fix for a specific problem.
Incision and Drainage
What it is: A dermatologist makes a tiny incision with a sterile needle or blade and gently drains the pus from a very large, soft cyst.
Warning: NEVER try this at home. You can push the infection deeper, cause severe scarring, and introduce new bacteria. A dermatologist does this in a sterile environment, often after injecting a steroid to ensure it drains completely and heals flat.
Photodynamic Therapy (PDT)
What it is: A treatment where a photosensitizing solution is applied to the skin, which is then activated by a specific wavelength of light.
How it works: It targets and destroys overactive oil glands and kills bacteria.
Effectiveness: Can be a good option for people who can't take oral medications. Results can be good but often require multiple sessions.
Side Effects: Can be painful during treatment and cause redness, swelling, and peeling afterward.
3. Supportive Topical Treatments
These won't cure a deep cyst on their own, but they are crucial for maintaining clear skin after the main fire is out.
Topical Retinoids (e.g., Tretinoin, Adapalene): These help keep the "pipes" clear by preventing new clogs. They are a cornerstone of long-term acne maintenance.
Topical Antibiotics/Benzoyl Peroxide: Help reduce bacteria and inflammation on the surface.
Pros and Cons of the Heavy Hitter: Isotretinoin
Given its central role in treating this condition, here’s a quick pros and cons list for isotretinoin:
Pros
Highest chance of long-term remission.
Targets almost all causes of acne.
Can prevent severe scarring.
"One-and-done" treatment course (usually 5-6 months).
Cons
Significant side effect profile.
Requires frequent blood tests and doctor visits.
Strict pregnancy prevention program required.
Can temporarily worsen acne at the start (acne flare).
Potential for rare but serious psychiatric and sexual side effects.
What About Diet and Lifestyle?
You might have heard that chocolate or greasy foods cause acne. The truth is more nuanced. There is no evidence that poor hygiene causes nodulocystic acne. However, research suggests that some dietary factors can influence inflammation.
High Glycemic Load Diets: Foods that spike your blood sugar quickly—like white bread, sugary drinks, and candy—may exacerbate acne. A diet rich in whole grains, vegetables, and lean protein can help keep inflammation in check.
Dairy: Some studies show a link between high dairy consumption (especially skim milk) and acne. It’s not a problem for everyone, but if you have severe acne, it might be worth trying a few weeks without dairy to see if it helps.
Stress Management: Easier said than done, we know. But because stress increases cortisol, which can increase oil production, finding healthy ways to manage stress—like exercise, meditation, or even just a good night's sleep—can be a helpful part of your overall skin care plan.
The bottom line: A healthy, balanced diet is good for your whole body, including your skin, but it's unlikely to be a standalone cure for this severe form of acne.
Living with Nodulocystic Acne: The Real-World Impact
It’s important to acknowledge that this condition is more than just skin deep. It hurts physically. And because it affects your face and body during your teenage and young adult years—a time when we are already self-conscious—it can take a serious toll on your mental health. Feelings of embarrassment, anger, and social anxiety are incredibly common.
If your acne is making you feel depressed or anxious, please talk to your doctor or dermatologist. Treating the acne can dramatically improve your self-esteem, and they can also point you toward resources for mental health support. You are not alone, and it’s not your fault.
Final Verdict
Nodulocystic acne is a tough, painful, and serious skin condition that requires serious treatment. It's not something you can scrub away or fix with a spot treatment from the drugstore.
The key takeaways are:
It’s a medical condition, often driven by genetics and hormones, not a reflection of your hygiene or habits.
See a professional. A dermatologist is your essential partner in creating a treatment plan to get this under control and prevent permanent scars.
There are powerful, effective treatments available. From targeted injections for a single cyst to life-changing courses of oral medication like isotretinoin, there is hope.
Be patient and kind to yourself. Finding the right treatment can take a few tries, and healing takes time. Focus on the long-term goal of clear, healthy skin and protect your mental well-being along the way.
Don't suffer in silence. Take that first step and book an appointment with a dermatologist. Your future self—with clearer, healthier skin—will thank you.
